Consolidation of Three Brooklyn Hospitals Restarts Mid-Pandemic, Staff, Community, and Advocates Push Back

In mid-March, a $700 million state plan to restructure three central Brooklyn hospitals was put on hold to ensure the institutions could accommodate the soaring number of coronavirus patients showing up at their doors.
Now, the plan to consolidate services and eliminate over 200 beds from Kingsbrook Jewish Medical Center while merging it with Interfaith Medical Center and Brookdale Hospital is again moving forward. But this time, a group of hospital staff, community members, and advocates is pushing back.

A petition, created by Kingsbrook nurses and titled Beds Not Bodybags: Do Not Close Kingsbrook Jewish Medical Center in the Middle of a Pandemic!, has garnered over 375 signatures, including at least 240 from Kingsbrook staff. Though hospital leadership says they are prepared for a potential second wave of coronavirus cases, the petition organizers worry that unless consolidation is delayed, the area’s already vulnerable medical institutions could again be overwhelmed.
“By closing this hospital before the second wave of the pandemic, which has the possibility of being worse than the first,” the petition reads, “Cuomo is working to ensure that even more Black Brooklynites will die.”
Reshaping Healthcare in Central Brooklyn
The hospital consolidation is part of Governor Andrew Cuomo’s Vital Brooklyn initiative, a $1.4 billion plan announced in 2017 that is intended to address health, social and economic disparities in several low-income Brooklyn neighborhoods.
Kingsbrook, Interfaith, and Brookdale are at the center of the initiative’s health component. The three independent hospitals serve large numbers of Medicaid and uninsured patients and have faced financial challenges for years. At the recommendation of a state-commissioned Northwell Ventures study, the hospitals’ management was centralized in 2018 under a not-for-profit entity called One Brooklyn Health, in the hopes that doing so would create cost-saving efficiencies.

The Governor then awarded about half the Vital Brooklyn funding to One Brooklyn in the form of grants. The money, according to a press release from the Governor’s office, will enable One Brooklyn to streamline services and to implement infrastructure and technology upgrades. It will also facilitate the transformation of Kingsbrook into a “medical village” focused on providing ”primary and specialty care, emergency services, and post-acute care services.”
That transformation requires the elimination of all of Kingsbrook’s 163 inpatient medical-surgical beds, along with dozens of additional beds for patients receiving treatment for coronary issues, traumatic brain injuries, and coma recovery.
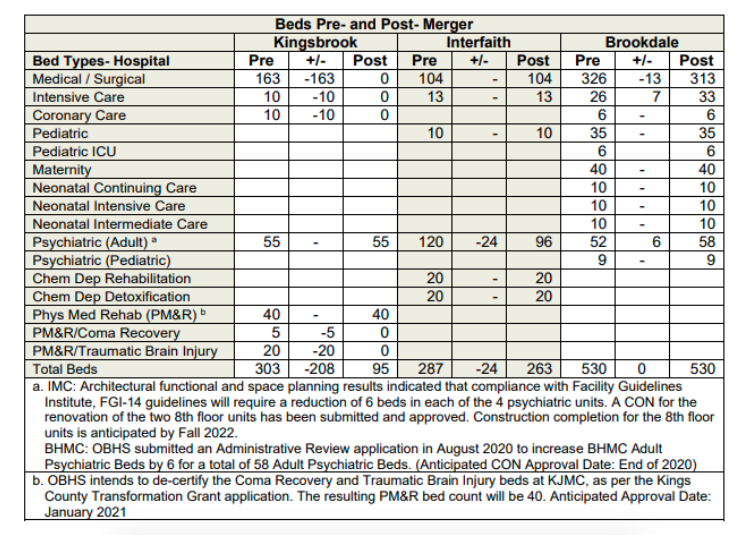
The deactivation of those beds was initially set to be completed by June 30th, but was paused when the pandemic began. Now, the planned completion date is January 1st. According to hospital staff, about 40 beds have been deactivated so far.
The goal, says LaRay Brown, One Brooklyn’s President & CEO, is to rationalize services across the system, and to recenter Kingsbrook around the type of primary and specialty care that could help patients stay healthy and avoid the overnight ER visits the hospital currently offers.
“We are committed to making Kingsbrook the hospital and healthcare campus of the future,” Brown said. “Which is less inpatient capacity, but many more outpatient services.”
COVID-19 Concerns
Some Kingsbrook staffers see things differently.
“I think that the pandemic has clarified that available hospital beds continue to actually be a very important part of the public health safety net,” said Julie Keefe, a Kingsbrook nurse who helped create the petition. “And it has really revealed that Cuomo and others have already gone too far with hospital closures and bed reductions in the boroughs.”
One Brooklyn’s data shows that occupancy rates of inpatient medical-surgical beds at Kingsbrook and Interfaith have hovered around 60% in recent years, while Brookdale has remained closer to 50% occupancy.
During the first wave of the pandemic, however, staff say all three hospitals were overwhelmed. Kingsbrook employees told the New York Times that the patient-to-nurse ratio at the hospital reached 20-to-1, far higher than the 4-to-1 ratio considered best practice. The patient-nurse ratio at Interfaith’s intensive care units, meanwhile, reached four times their recommended 2-to-1 level.
“All of these hospitals were inundated with people,” said Jacinda Browne, a clerk at Kingsbrook who signed the petition.
In documents submitted to the state health department in August, One Brooklyn estimated that, when Kingsbrook closes, “approximately one third of the utilization will be retained at IMC and/or Brookdale, while the other utilization will either be captured by other area hospitals or will not materialize.”
Brown said she has been in close contact with the leadership at nearby Health + Hospitals / Kings County, a city-run institution, as the consolidation has progressed. But Kings County Hospital was itself flooded with coronavirus patients in the spring, and faces its own financial challenges.
Health + Hospitals / Kings County did not respond to a request for comment.
In any case, Brown says she is confident Brookdale and Interfaith have the capacity to handle a second wave of coronavirus cases. At the peak of the spring outbreak, she said, One Brooklyn hospitals admitted about 500 COVID-19 patients at a time; 300 who had tested positive, as well as 200 patients with severe symptoms awaiting test results.
By adding more beds to existing inpatient areas and converting beds currently designated to treat substance abuse, Brown estimates the two hospitals will have room for up to 540 COVID patients. And Kingsbrook will retain an outpatient emergency department that can treat symptomatic patients who do not require overnight stays.
“I have absolutely no concern that we can activate the necessary number of beds,” said Brown.
Brown says the greater challenge for One Brooklyn is ensuring sufficient staff are available to activate those beds. At a State Department of Health hearing last month, she suggested that National Guard staff and resources, which in the spring were deployed to field hospitals in Manhattan, should instead be directed to community hospitals in the outer boroughs.
Nevertheless, the inequity in bed counts across the city remains stark. Borough-wide, there are currently 2.2 hospital beds for every 1,000 residents in Brooklyn, far fewer than the 6.4 beds per 1,000 residents that exist in Manhattan.
A Challenging Healthcare Landscape
The drastic difference in the number of beds in each borough, advocates say, is indicative of a broader inequality that exists throughout New York’s healthcare system.
43 hospitals across the state have closed since 2003, including at least a dozen in the city, and New York’s total bed count has fallen from 74,000 to 53,000. The majority of the closed institutions were, like those managed by One Brooklyn, so-called safety-net hospitals that disproportionately serve the uninsured, Medicaid, and other vulnerable populations.
“The reason these hospitals have financial difficulties is not that they are mismanaged or that people in those communities do not need care,” said Dr. Steve Auerbach, a member of the Executive Committee of Physicians for a National Health Program’s New York chapter, which signed on to the Kingsbrook petition. “It is because of how our healthcare system, in general, is financed, in a way that systematically favors the wealthy.”
Auerbach’s organization advocates for a single-payer health program at the federal and state level, which could address such financing problems. But he and other activists point to a number of other policy decisions they say exacerbate the disparity. In 1997, for example, New York State weakened its protocols for regulated hospital reimbursement rates, allowing hospitals in wealthy areas to demand higher rates from the private insurers that serve many of their patients, which hospitals in poorer, more Medicaid-dependent neighborhoods don’t have the leverage to do.
Even programs intended to close the gap can have the opposite effect. A prime example, advocates say, is the way in which the state allocates its $1.13 billion in Indigent Care Pool (ICP) funding each year.
The ICP program, which draws from a mix of federal and state funds, is intended to stabilize hospitals that serve low-income communities. But rather than direct the money exclusively to safety-net institutions, as all other states do, New York State distributes it to a much broader selection of hospitals, including many that do not serve significant numbers of low-income people. A recent report by the anti-poverty group Community Service Society found that, in the past 20 years, New York’s safety-net hospitals received about $13.4 billion less in ICP funding than they would have if they had been located in any other state.
The pandemic has not made things easier. In April, the state passed an austerity budget that included a $400 million reduction in Medicaid payments to hospitals, alongside other cost-cutting changes that could hit safety net institutions particularly hard.
“The governor makes across-the-board cuts in Medicaid reimbursement,” said Judy Wessler, former Director of the Commission on the Public’s Health System, an advocacy organization. “If you have a hospital with a large endowment and lots of privately-insured patients, you can do okay. Safety-net hospitals have lots of patients with Medicaid. And the thing about Medicaid reimbursement is that it’s already far below what private insurance would pay.”
The structural challenges are such that, even with the savings accrued through consolidation, One Brooklyn will remain in the red for the foreseeable future. The organization’s financial projections estimate that, in three years, One Brooklyn will register a net loss of $69,127,457. The gap will be filled, as it has in the past, by state support.
Unions And Elected Officials Still Support The Plan
Several elected officials and union leaders, as well as Ms. Brown herself, said they recognized the underlying funding issues. But they continue to believe the One Brooklyn consolidation plan is the right path.
“I don’t think that we should be either-or,” said Senator Zellnor Myrie, whose district includes Kingsbrook, and who was elected in 2018, after much of the planning surrounding Vital Brooklyn had been completed. “The ultimate barometer of what is going to be successful is what allows our healthcare system to serve our constituents. And I think given the reality of the current financial situation, it’s important for us to have all options on the table.”
Myrie said his conversations with One Brooklyn and union leadership had reassured him that the consolidation did not pose a public health risk, and expressed concern at what he sees as confusion or misinformation circulating within some communities.
“Without question, there’s a breakdown in communications,” Myrie said. “It might be helpful for us to all be in the room together – the proverbial room – to ensure that we’re communicating with each other. Because if there’s not cause for panic, this is really not an ideal time to insert it.”
Myrie’s counterpart in the Assembly, Diana Richardson, was more blunt.
“Some people cause havoc and fearmongering in the community unnecessarily, as a result of bad information,” Richardson said at a virtual Civic Minded community meeting last month. Richardson has organized community discussions about Vital Brooklyn and produced a report that was incorporated into the plan.
“Kingsbrook Jewish Medical Center is not closing,” she told meeting attendees. “Will there be a transformation by way of Vital Brooklyn at Kingsbrook Jewish Medical Center? Yes, absolutely.”
Both the New York State Nurses Association and 1199 SEIU, which were closely involved in the plan’s development and organized information sessions for members in partnership with One Brooklyn leadership, remain strongly supportive.
In a statement, NYSNA called the merger “an extraordinary investment in communities historically underserved.” The Association represents 280 nurses working at Kingsbrook and 170 working at Interfaith and says they will all remain employed after the consolidation. 1199 SEIU, which represents many healthcare workers employed by One Brooklyn, declined to comment on this story.
Those who signed the petition remain unconvinced and say the distinction between closure and transformation is little more than a semantic one when so many hospital beds are at stake.
“I can’t understand why the elected officials would be so comfortable with the idea of reducing the amount of medical services in their district,” said Victor Jordan, a Brooklyn resident and member of nearby Community Board 17 who signed the petition. “I’m baffled.”
Nevertheless, without formal opposition, the consolidation continues.
Late last month, a committee of the state’s Public Health and Health Planning Council, which advises the Department of Health on construction projects and service changes in healthcare facilities, voted to recommend approval of One Brooklyn’s application to formally merge its hospitals into one corporate entity. The full Council will take up the application on October 8th, and its recommendation will then go to the New York State health commissioner, Howard Zucker, who is the final decision-maker.