Geriatrics House Calls Program At Brooklyn Hospital Is Building Bridges In Health Care (Part I)

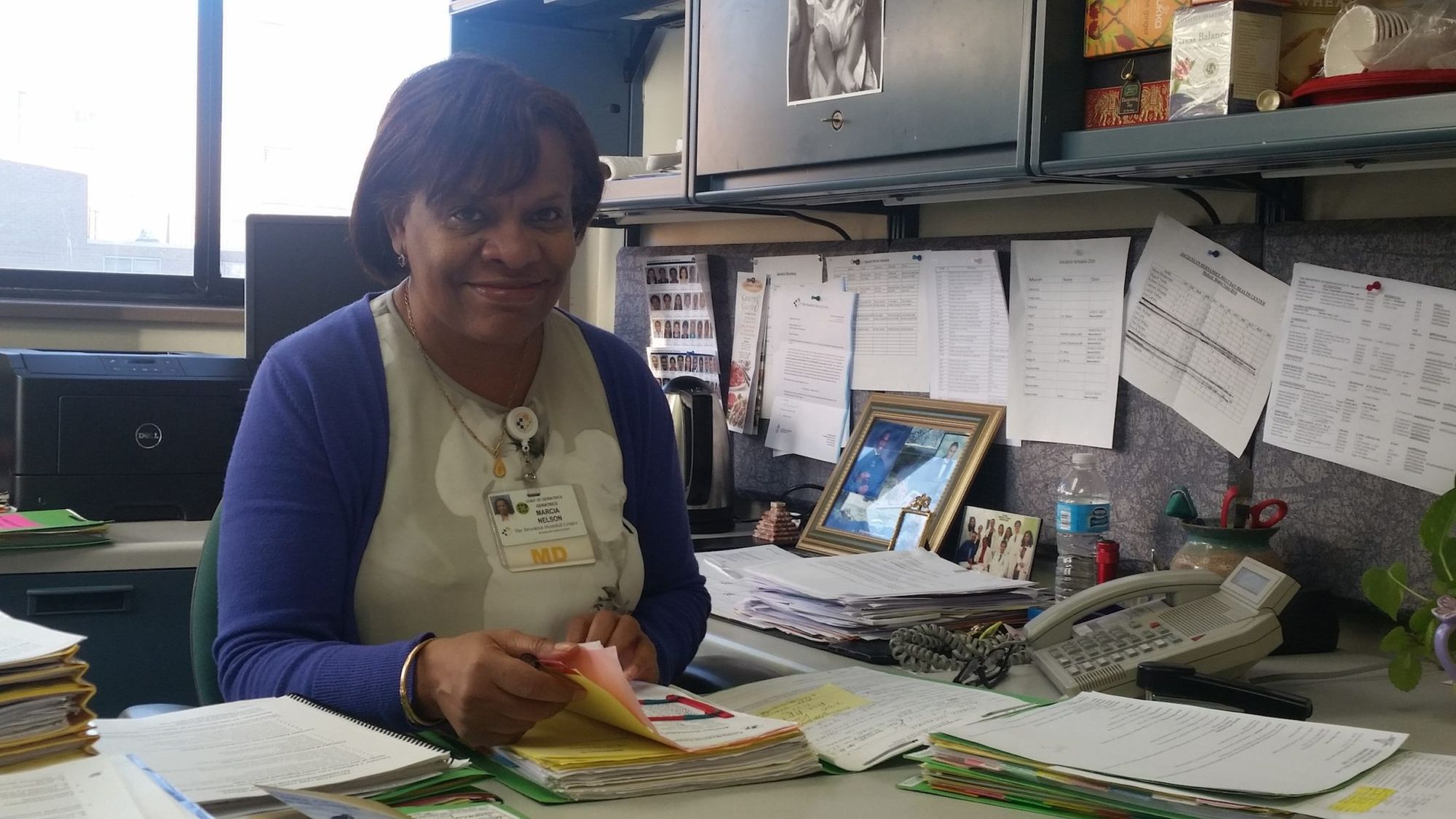
Dr. Marcia Nelson is so reassuring and friendly, patients don’t even realize that their casual conversation about how they’ve been feeling, how comfortable or uncomfortable their beds and chairs are, and what they’ve been eating counts as giving their medical history. But that’s the point.
Unlike a tedious paper or touch-screen iPad questionnaire, house calls rely on the power of observation.
“Geriatrics is total care,” explained Nelson, who is the chief of geriatrics at Brooklyn Hospital Center, where she leads a team of three geriatricians (one of them focusing on palliative care), two nurse practitioners, one social worker, and one program coordinator.
“Visiting patients at home is a unique opportunity to glimpse their life and situation: if they have old medication, clutter, a potential for falls, mobility, proper temperature, and things like that,” she said. “Then we’re able to implement more treatment services that they need and are okay with.”
Examples of services she can order? More home care, Pills on Wheels, lab tests and x-rays, and food delivery from nonprofits such as In God’s Love We Deliver.
“For example, if you have a cough, sputum, and a fever, we can send a lab tech to take an X-ray in your home and contact the pharmacy, where either the family member picks up the meds or we send it to you. The whole point is to provide the care you need.”
“The Future Of Medicine”
House calls may sound like something out of the past, from a less complicated time, or only doable in small communities where people know and live next to their doctors — not in urbane, metropolitan areas like Brooklyn. But increasingly, that isn’t the case.
Although [these] practice may harken back to the country doctor of decades past, it could be the future of medicine. In 2013, about 2.6 million Medicare claims were filed for patient home visits and house calls. That’s up from 2.3 million visits in 2009 and 1.4 million visits in 1999, according to Medicare statistics.
The trend is expected to accelerate as baby boomers grow older. One in 20 people over the age of 65 is homebound in the U.S., according to a study published in July in JAMA Internal Medicine.
However, at the moment, house calls only make up less than 1 percent of doctor-patient encounters, according to cardiologist and author Sandeep Jauhar in a New York Times opinion piece. That is compared to “about 40 percent” of interactions before World War II. Why? Cost — of travel and time spent with each patient compared to how many can be seen when patients come to the hospitals or clinic.
But as Brooklyn Hospital’s Dr. Nelson notes, there is also the cost to patient health to consider.
“The care of the elderly is different from the care of the average adult. It’s specific and very gratifying. I learn a lot from patients,” she explained. “They need someone to speak for them, to be their advocate, to improve their quality of life. It feels good to have someone come in, discuss the problem they have, and leave with a solution. People can be emotional and need encouragement, too — it’s not just medical.”
She also pointed out that if cost is the measure, then prevention and the reduced cost of hospitalization far outweighs the cost of travel.
“I think [house call] programs will become more common as hospitals try to decrease the rate of hospitalization. It’s expensive to see patients in the hospital, where you have to have cleaning people, dietitians, nurses,” said Nelson. “It’s much less expensive in a home.”
Dr. Jauhar concurred, writing that “if we revived the house call, the overall savings to the health care system, not to mention the impact on patient care, would be enormous.”
Here in Brooklyn, there are only a few non-private, small hospital-based house call programs that operate by request and referral, and sometimes only with specific services: the one at Brooklyn Hospital, one at NYU-Lutheran Medical Center, and one out of New York Methodist. The rest are run through either private agencies, which charge fees for enrollment, or small community-based organizations that serve a targeted group of people.
This is the first in a series of articles we are doing on house calls and the Brooklyn Hospital Geriatrics Department’s house calls program. Our next installment will follow the patient perspective.